Medetomidine in Illicit Drugs
Public health officials have recently begun to sound the alarm about a new street drug that may be responsible for overdose surges in a few large U.S. cities. Manufacturers typically add medetomidine to fentanyl and other illicit recreational substances. As a result, many people who are harmed by it may not even realize they’ve taken it.
What is Medetomidine?
Medetomidine is a veterinary sedative and anesthetic. In the U.S., it has earned approval from the Food and Drug Administration (FDA) to sedate dogs for certain procedures.
The FDA has also approved a version of medetomidine called dexmedetomidine. This is authorized to be used on human patients who need to be sedated while on a mechanical ventilator or prior to surgery.
Illicit Drugs Laced with Medetomidine
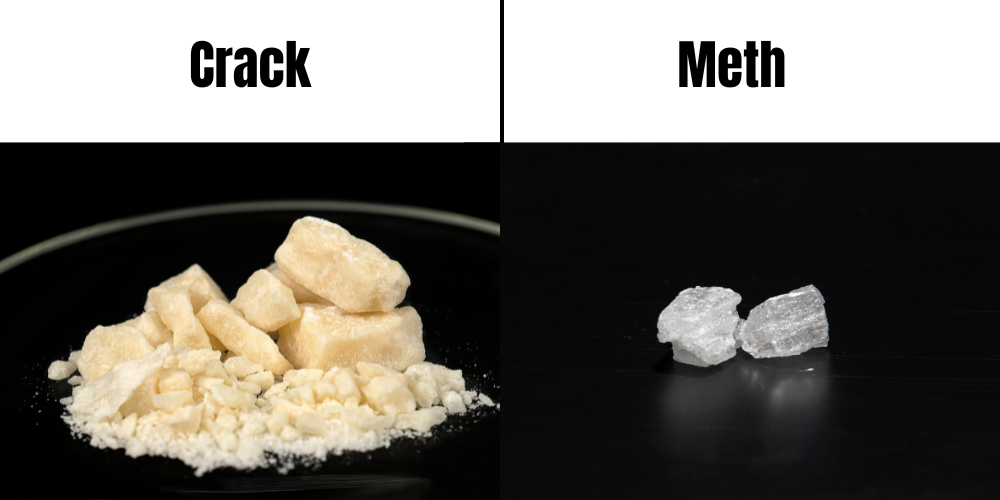
Fentanyl and heroin are the two illicit drugs most likely to be contaminated with medetomidine. Some sources have also detected medetomidine in samples of cocaine. However, this doesn’t seem to be nearly as common as opioid and medetomidine combos.
When abused on their own, fentanyl, heroin, and cocaine can all put people at risk for serious negative outcomes, including overdose and death. Combining them with medetomidine significantly increases their danger. This danger may be magnified by the fact that most people don’t realize that the drug they’re taking contains this undisclosed ingredient.
In a June 3, 2024, CBS News segment, an employee of the Philadelphia Department of Health said that the department detected medetomidine in samples of street drugs that also contained fentanyl and xylazine.
The combination of fentanyl and xylazine is often referred to as “tranq.” According to one source in the CBS News segment, some people are referring to the fentanyl-xylazine-medetomidine combination as “rhino tranq.” However, another experts have said that they had not heard that term.
Regardless of their names, the recent surge in illicit street drugs mixed with medetomidine suggests that the nation may face another devastating increase in overdose deaths.
Dangers of Medetomidine
A June 2, 2024, feature on National Public Radio (NPR) reported that medetomidine was involved in “mass overdose outbreaks” in Chicago and Philadelphia during the previous two months. In Philadelphia, according to the NPR feature, medetomidine-related overdoses caused 160 hospitalizations over a four-day period.
In addition to the risk of overdose, someone who takes medetomidine in a non-medical setting may also be in danger for a variety of other problematic outcomes, including:
- Slowed heart rate and breathing
- Low body temperature
- Dangerously low blood pressure
- Elevated blood glucose level
- Excessive urination
- Vomiting and diarrhea
- Twitching
- Easing of anxiety
- Hallucinations
- Delusions
- Paranoia
How to Help Somone Who Is Overdosing
Common signs of medetomidine overdose include:
- Constricted (pinpoint) pupils
- Extremely slow or shallow breathing
- Faint pulse
- Disorientation
- Difficulty remaining awake
- Loss of consciousness
- Cool, clammy skin
- Blue or purple color near lips or fingertips
Anyone who exhibits these signs after using medetomidine or another drug needs immediate medical help. If you are with someone who is in the midst of a medetomidine overdose, take the following steps:
- Call 911 or otherwise summon the closest emergency responder in your area.
- If you have naltrexone (Narcan), administer it to the person who has overdosed.
- If the individual is awake, help them into a seated position in a comfortable chair.
- If the individual is unconscious and cannot be awakened, place them on their side. Do not put them on their back (to reduce the risk of choking if they begin to vomit).
- Cover the person with a blanket to keep them warm.
- Remain with the person until the emergency responders arrive.
- Be prepared to tell the emergency responders as much as you know about what substances the person took, how much they took, and what overdose signs they exhibited.
Also, here are a few important notes about naltrexone (Narcan):
- Though Narcan can reverse an opioid overdose if administered in time, it cannot reverse a xylazine or medetomidine overdose.
- Since people who ingest medetomidine have usually taken it in combination with an opioid, most trusted sources advise giving Narcan to someone who has overdosed.
- However, even though the person may appear to be revived and out of danger after receiving Narcan, any medetomidine in their system may still be harmful to them.
- This is why you should always call 911 first, even if you have Narcan with you. A person who has overdosed on an opioid combined with medetomidine needs a thorough assessment by a qualified healthcare provider, even if they seem OK after receiving Narcan.
Get Help for Drug Addiction at Sanctuary Treatment Center
Sanctuary Treatment Center offers a full continuum of care to help adults who have become dependent on opioids or any other addictive substances. We also serve patients whose struggles with addiction are accompanied by anxiety, depression, PTSD, and certain other co-occurring mental health concerns.
Programming options at our addiction treatment center in Los Angeles, California, include detoxification (detox), inpatient rehab, and outpatient care. Our team of experienced professionals will work closely with you to assess your needs, determine which level or levels of care are right for you, and select the therapies and support services that will best prepare you to achieve successful, long-term recovery.
When you’re ready to end your compulsive substance abuse for good, the Sanctuary Treatment Center team is here for you. To learn more or to schedule a free assessment, please visit our Contact page or call us today.